Cesarean Birth Recovery Guidelines
Delivering via Cesarean, or C-section, is a common way many mothers bring their babies into the world. However, the recovery and physical changes that follow can be profound. Pregnancy itself brings significant transformations to the body, including shifts in posture, weight distribution, and pelvic floor dynamics. A C-section adds another layer of impact due to the abdominal incision, which involves cutting through six layers of tissue and muscle. This can lead to core weakness, scarring, and altered sensation around the area.
While both C-section and vaginal deliveries can result in core weakness and changes in center of mass, a C-section uniquely affects the body with scarring, numbness, and reduced sensation around the incision site. Scar tissue may sometimes create tightness, affecting mobility and comfort, and the pelvic floor muscles can be impacted by the weight and pressure of pregnancy, potentially leading to issues with bladder control or core stability.
This guideline is designed to provide you with safe strategies to rebuild strength and promote long-term pelvic health, so you can return to your activities feeling confident and supported. It focuses on gradually restoring strength and addressing changes in the pelvic floor, abdominal muscles, and overall body mechanics.Summary of body changes:
The three main components of postpartum recovery are:
Recovery of proper breathing
Muscle function including motor control, strength and flexibility
Organ position
It took your baby nine months to grow, and you also changed during that time. Recovery will take time as well. During your pregnancy, your body underwent skeletal changes, and your joints became looser. Throughout your recovery process, exercise should focus on re-stabilizing these joints while restoring core strength.
Ribs: Your rib cage expands by about 10-15 cm in circumference. To avoid rib pain and improve the efficiency of your abdominal wall, retraining your breathing pattern can be helpful.
Pelvis: Your pelvis was preparing to open to allow your baby to grow and pass through. Regardless of how you delivered your baby, your pelvis needs support to return to a normal, stable state in order to reduce back, hip, and pelvic pain..
Organ position: Your baby filled a large space in your belly, so now all your organs need to migrate back to their original positions. This process can take about six weeks. You can support the return of your organs by following precautions, using binding techniques, and restoring your core strength.
Cesarean Scar Recovery
For anyone who has had a cesarean (C-section) delivery, this involves an incision through the abdominal wall. These scars are typically located either horizontally above the pubic bone or vertically below the belly button. The incision goes through six different layers of the abdominal cavity, with stitching done at the uterus, sometimes the rectus abdominis muscle (6-pack muscle), and the skin. Returning to a general exercise program is generally safe once the incision has healed, and addressing the scar can help improve abdominal engagement, flexibility, and pressure control. Here are some guidelines for scar healing:
First 2 Weeks: This is the initial phase of healing, where you may experience swelling, redness, or tenderness. Icing can help manage these symptoms.
4–6 Weeks: Deeper tissues under the skin are healing, even though you can’t see them; remember, the incision went through six layers. You may experience numbness or decreased sensation around the scar.
3–6 Months: The scar tissue continues to mature and remodel, but tightness and numbness around the scar are common.
6–12 Months: By this point, the scar is typically fully healed, although numbness and sensitivity may persist.
Healing time varies based on factors like skin type, physical activity level, and any complications. Gentle massage starting around 3 weeks, about 2–3 inches above the scar, can help reduce swelling, tenderness, and tension.
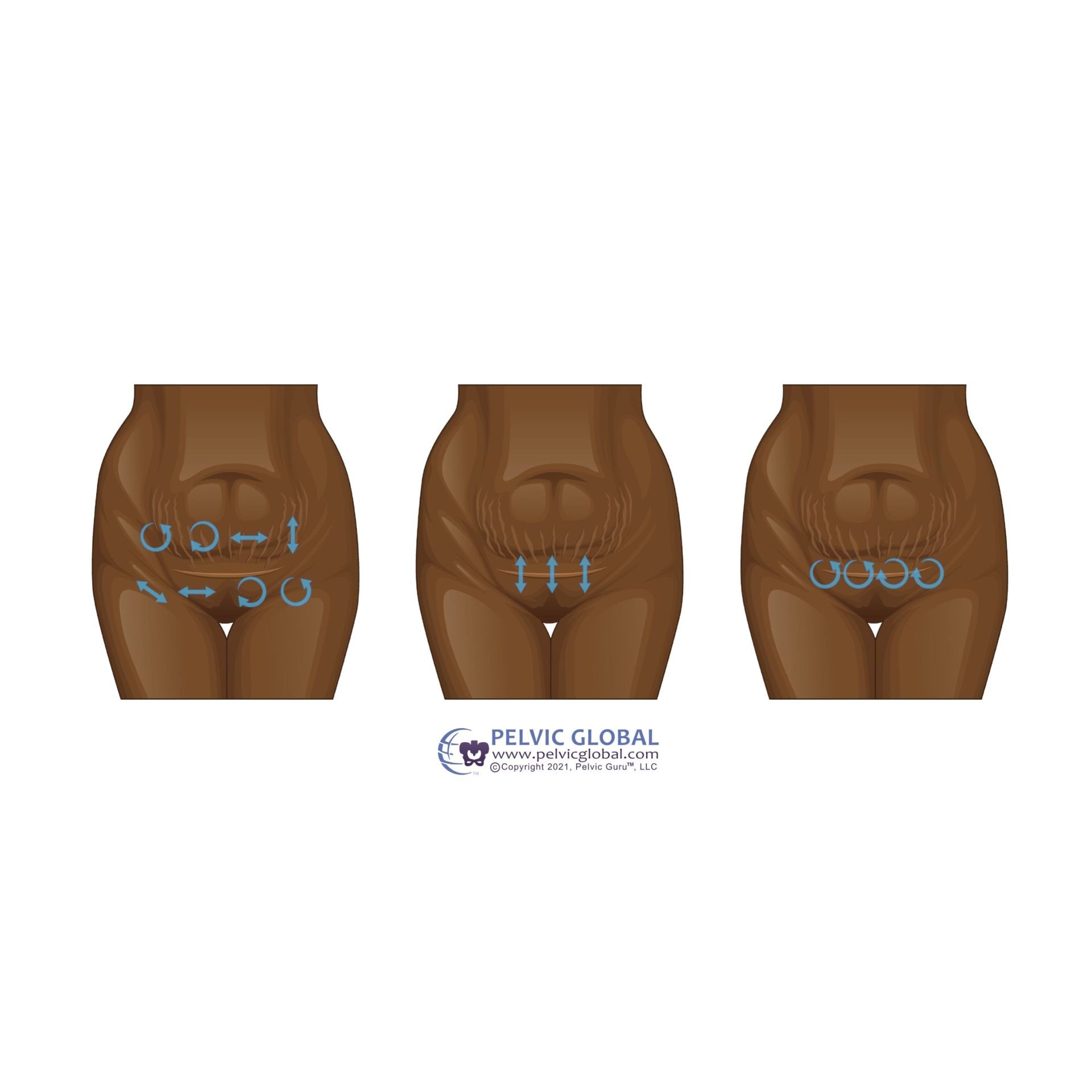
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Tips for Scar Massage:
Place a towel between your skin and the scar, then apply ice 2–3 times per day for 20 minutes.
Keep the incision dry to reduce the risk of infection.
Spend time lying flat to gently stretch the incision, helping you feel less discomfort when standing.
Avoid wearing tight pants or underwear. Cesarean-specific underwear can provide support during initial healing.
Read for more tips on recovery from a cesarean scar, click here
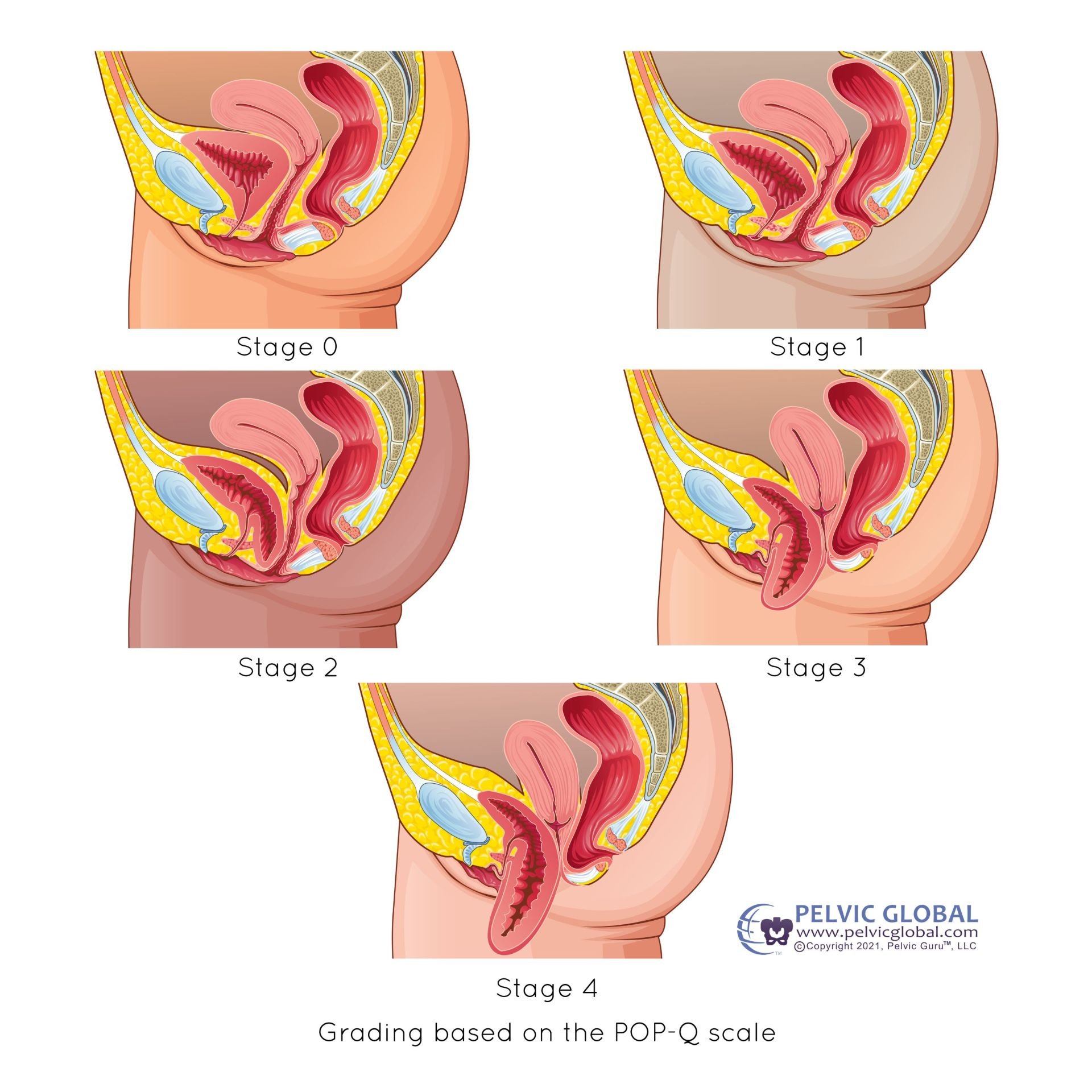
Pelvic Organ Prolapse
Pelvic organ prolapse (POP) is the descent of vaginal organs that creates a bulge or pressure at the vaginal opening. This occurs due to weakening of the support structures, such as ligaments, the health of vaginal tissue, and pelvic floor muscles. POP is common after vaginal delivery.
A key difference between identifying a prolapse immediately after childbirth versus five years later is the potential for improvement within the first year postpartum. Typically, physical therapy cannot change the stage of a prolapse, but there’s more opportunity for improvement in the immediate postpartum period.
If you'd like to learn more about pelvic organ prolapse, I’ve written several blogs, which you can find here:
The Low Down On Pelvic Organ Prolapse
Overcoming the Frustrations of Bladder Prolapse
Stages of a Cystocele (bladder descent)
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Tips to Manage Pelvic Organ Prolapse:
Avoid straining during bowel movements.
Use the "blow while you go" technique when lifting your baby (see core recovery for details).
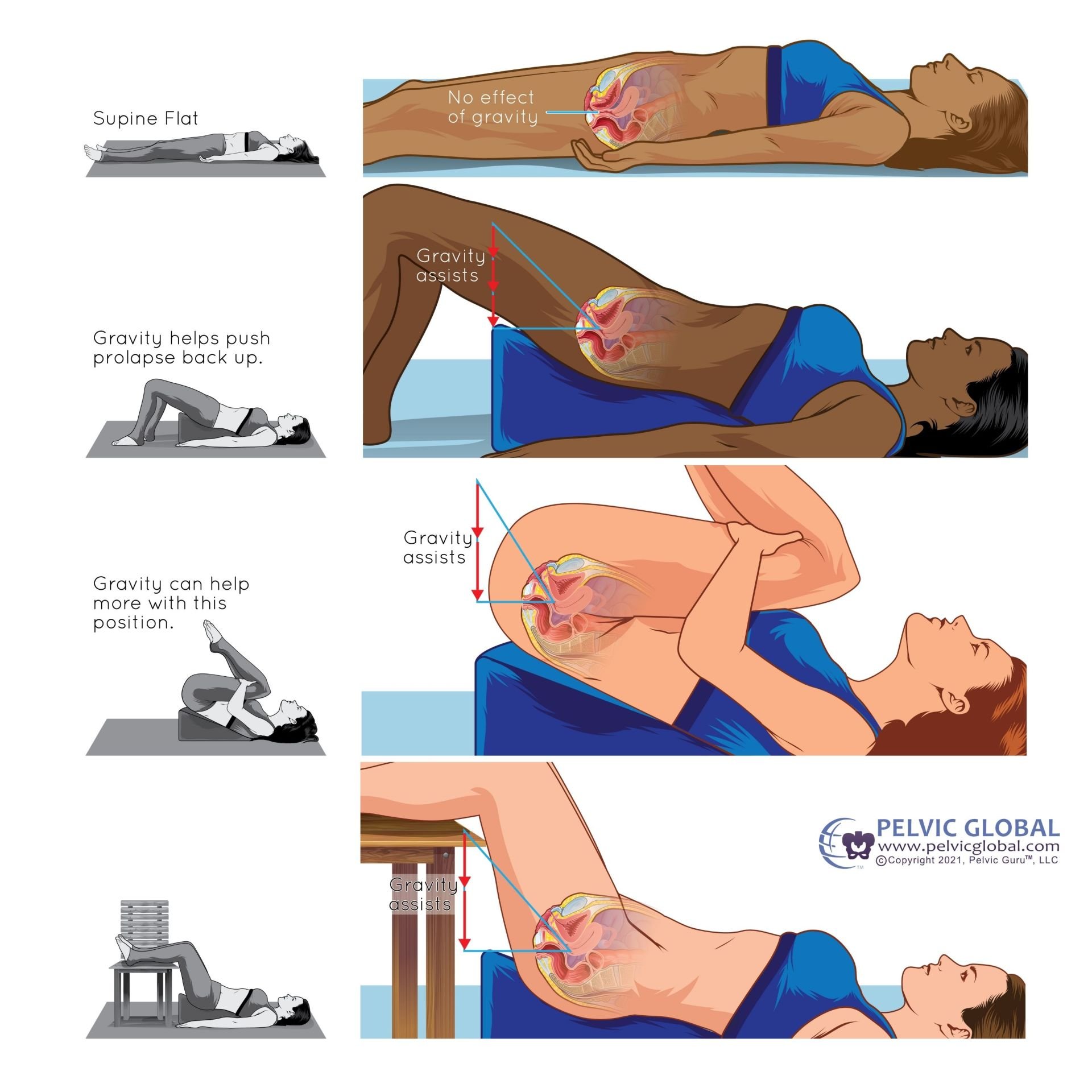
Take pelvic rest: if the pressure feels too heavy, elevate your feet—see the image for suggestions.
Schedule a pessary fitting. A pessary is a temporary device inserted into the vaginal canal to support the prolapse. It can help manage your symptoms and improve muscle engagement.
Pelvic Rest Position Suggestions:
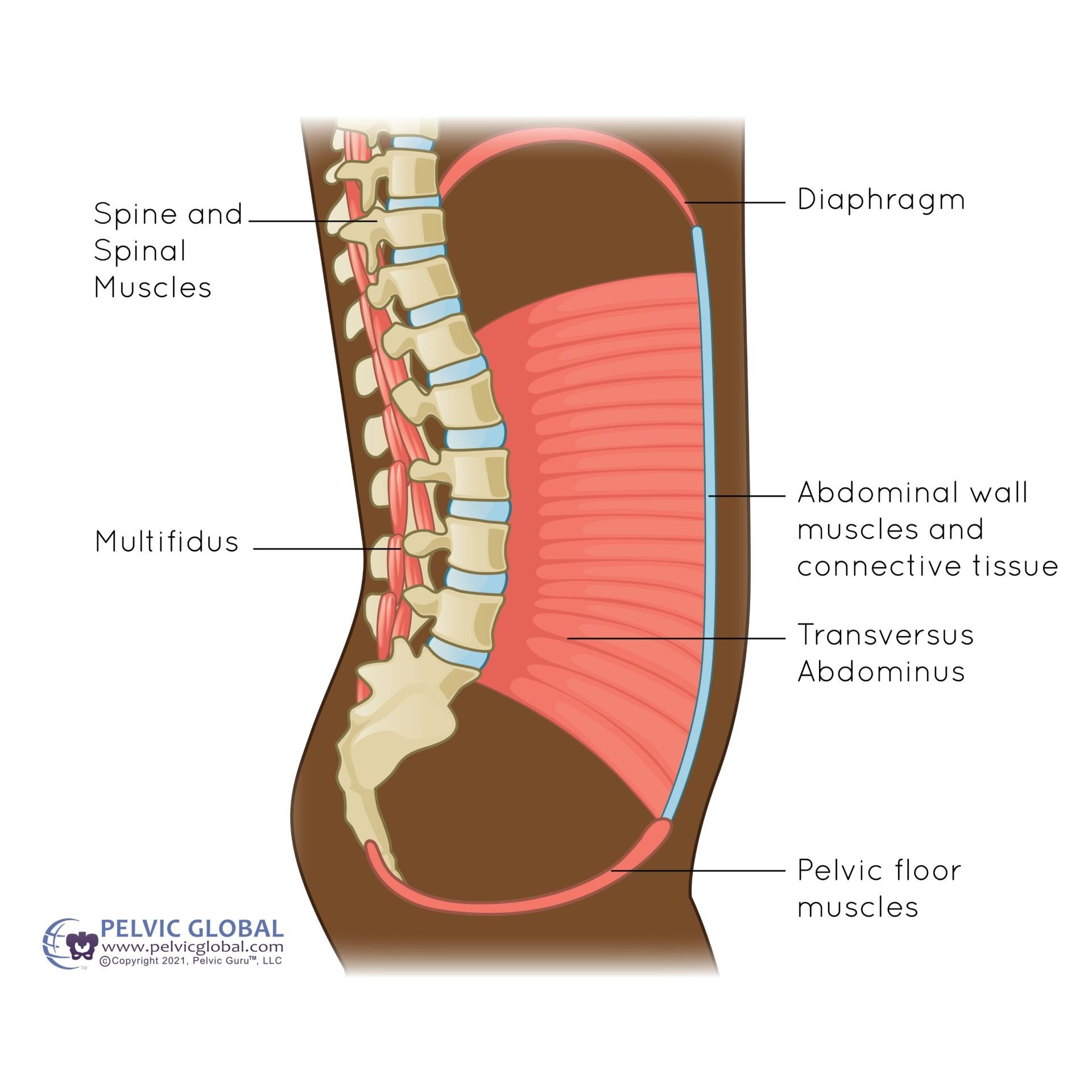
First, let’s define what the core is. Many people think the core refers solely to the lower abdominal wall, often using the cue “pull your belly button to your spine.” In reality, the core encompasses much more, including the entire abdominal wall, diaphragm, deep spinal muscles, and pelvic floor muscles. Refer back to the page on what happens to your body during the postpartum period. The abdominal wall takes a significant hit and needs attention to recover.
Immediate Tips for the Core Canister:
Consider relaxing with your baby for about two weeks! This time allows you to heal and gives your body a break from the significant event you just experienced. If possible, focus on your baby while the people in your life help with laundry, dishes, cleaning the house, cooking dinner, or taking care of the baby when you need to get up from a chair or bed.
Use the strategy of “Blow While You Go” when getting up from a chair, picking up or putting down your baby, or lifting a heavy car seat. To practice this technique, blow out through a skinny straw each time you pick up your baby. See the image below to understand how the entire system works together. The exhale helps activate the pelvic floor, abdominal and spinal muscles, and contracts the diaphragm.
Core Muscle Recovery:
The Core Canister
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Pay attention to your posture! First, there is no such thing as perfect posture; your body naturally wants to move and change. Each time you hold your baby, try to vary your posture and switch up the side you hold them on.
Exercise is best managed with the guidance of your physical therapist, who can monitor your blood pressure and ensure you feel safe during the early postpartum period. Consulting with a physical therapist doesn’t have to be overwhelming. It can start with an initial consultation to provide tips, exercises, and an overview of how you’re feeling. Follow-up sessions can be scheduled weekly or monthly for check-ins. The goal is to coach and guide you through your recovery while accommodating your less flexible schedule.
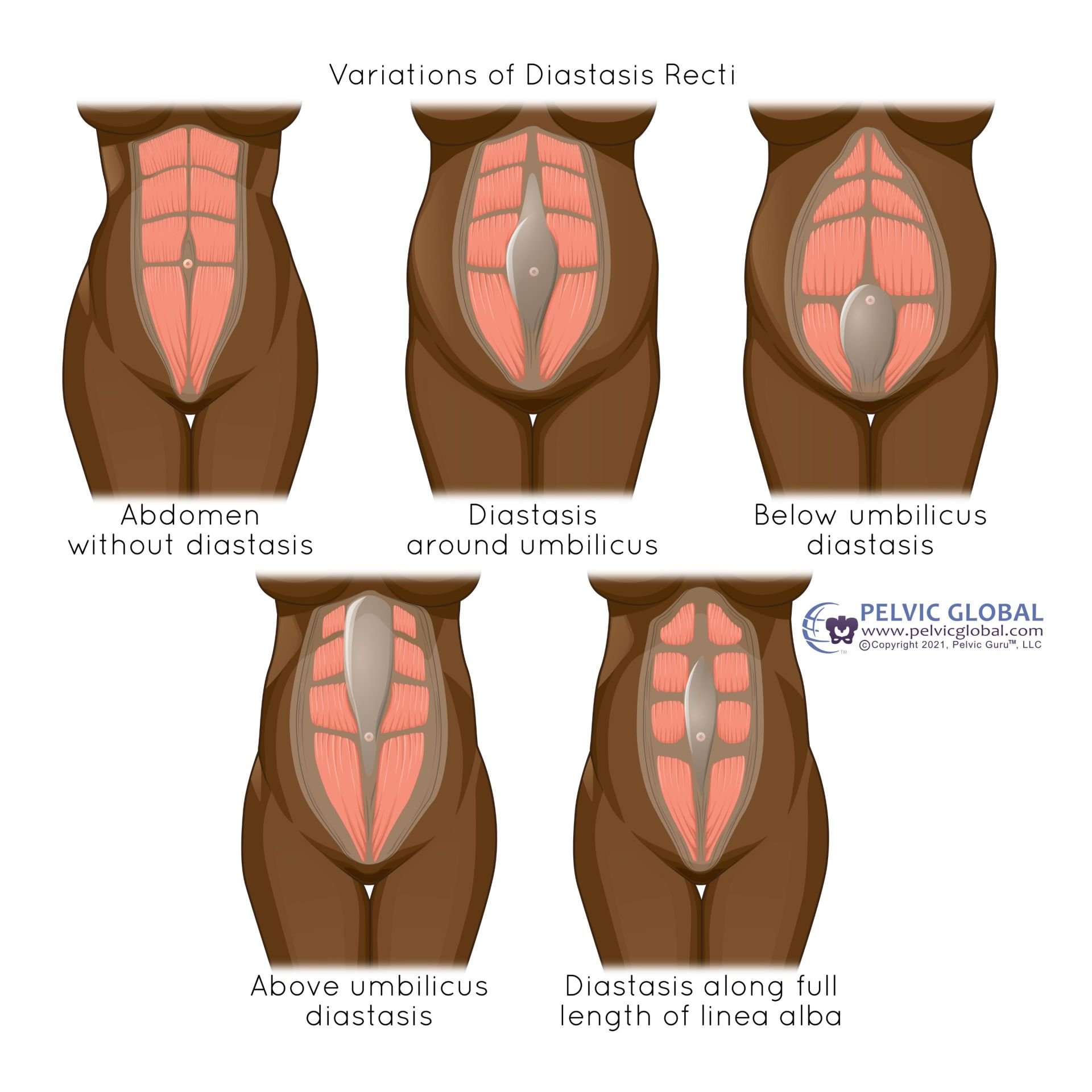
Diastasis Rectus Abdominis (Abdominal Seperation)
Diastasis Rectus Abdominis (DRA) is the separation of the linea alba, the connective tissue that divides the two sides of the 'six-pack' muscle. Some key facts about DRA include:
It’s a common condition.
It occurs when there’s rapid weight gain in the abdominal area, such as during pregnancy, though you don’t need to be pregnant to experience DRA.
You cannot prevent DRA, and nothing you did caused it.
DRA typically develops in the third trimester.
Losing weight won’t fix DRA.
There are no 'bad' exercises for DRA; the focus should be on building strength, improving function, and managing pressure in the abdominal wall.
Lifting and caring for your baby won’t make DRA worse.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
Tip for DRA (abdominal seperation)
Perform a log roll when getting into and out of bed to help prevent doming or bulging
Use “Blow before you go” techniques when picking up baby or during transtional movements like getting out of bed
To Bind or Not to Bind:
An abdominal binder can help support your core during the early weeks postpartum. You can wear a binder whether or not DRA is present. Remember, your abdominal wall has been stretched and essentially 'popped' like a balloon when you delivered your baby. Your abs may need some extra support as you care for your growing baby!
Tips for wearing a binder:
Wear the binder while moving around especially if you are doing house work, laundry, long walks.
It may be uncomfortable to sit, this is not recommended
Wearing a binder will not weakening your muscles.
Things that are “not normal”
…but can happen – if you experience any of these, please consider seeing a pelvic physical therapist sooner rather than later. It is easier to fix these problems now!
Pain
Pain with intercourse, bowel movements, urination, sitting, walking, moving in bed, picking up your baby, etc.
Abdominal pain, hip pain, low back pain, pubic pain, pelvic pain, tailbone pain, thoracic pain, shoulder pain, neck pain.
Anything falling out of your vagina or a feeling of heaviness in your vagina.
Burning or itching around your vaginal opening or in your pelvis.
Sensitive scars.
Urine leakage – even a little bit! – Should return to normal within 6 weeks.
Fecal leaking/Constipation.
A split in your rectus muscles, or a pooch when you move.
Something just doesn’t “feel right”.