Section 2:
Changes to Your Body Post Surgery
Pelvic organ prolapse (POP) surgery can bring about a range of changes in the body, both immediately after the procedure and over the long term. These changes are influenced by the type of surgery performed, the extent of the prolapse, and individual factors.
Here are the key changes that typically occur:
Structural Changes:
Restoring your anatomy: Organs are surgically placed back into the correct position.
Result: A reduction of a bulge and re-enforces pelvic support increase.
Strong Support Structures: Surgically intervention improves stability and function of the pelvic floor organs.
Result: A reduction in symptoms such such as heaviness or pressure. Note: You can still have about a 30% of Urinary Leakage post surgery which can be initially treated with Pelvic Floor Physical Therapy.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Pelvic Floor Muscle Changes:
Pelvic floor muscle activation: With reduction of pressure off the pelvic floor muscles, you have an opportunity to activate and strengthen your muscles in an optimal approach. Initially you may feel weak or have altered sensation.
Result: Pelvic Floor Physical Therapy can help improve muscle activation.
Potential muscle tension: Muscle tension may be present due to overcompensation when prolapse was present. You may also feel tension due to scar recovery based on your surgery.
Result: Potential discomfort with pelvic exams or returning back to penetrative intercourse. Pelvic Floor Physical Therapy can help improve muscle tension and scar mobility.
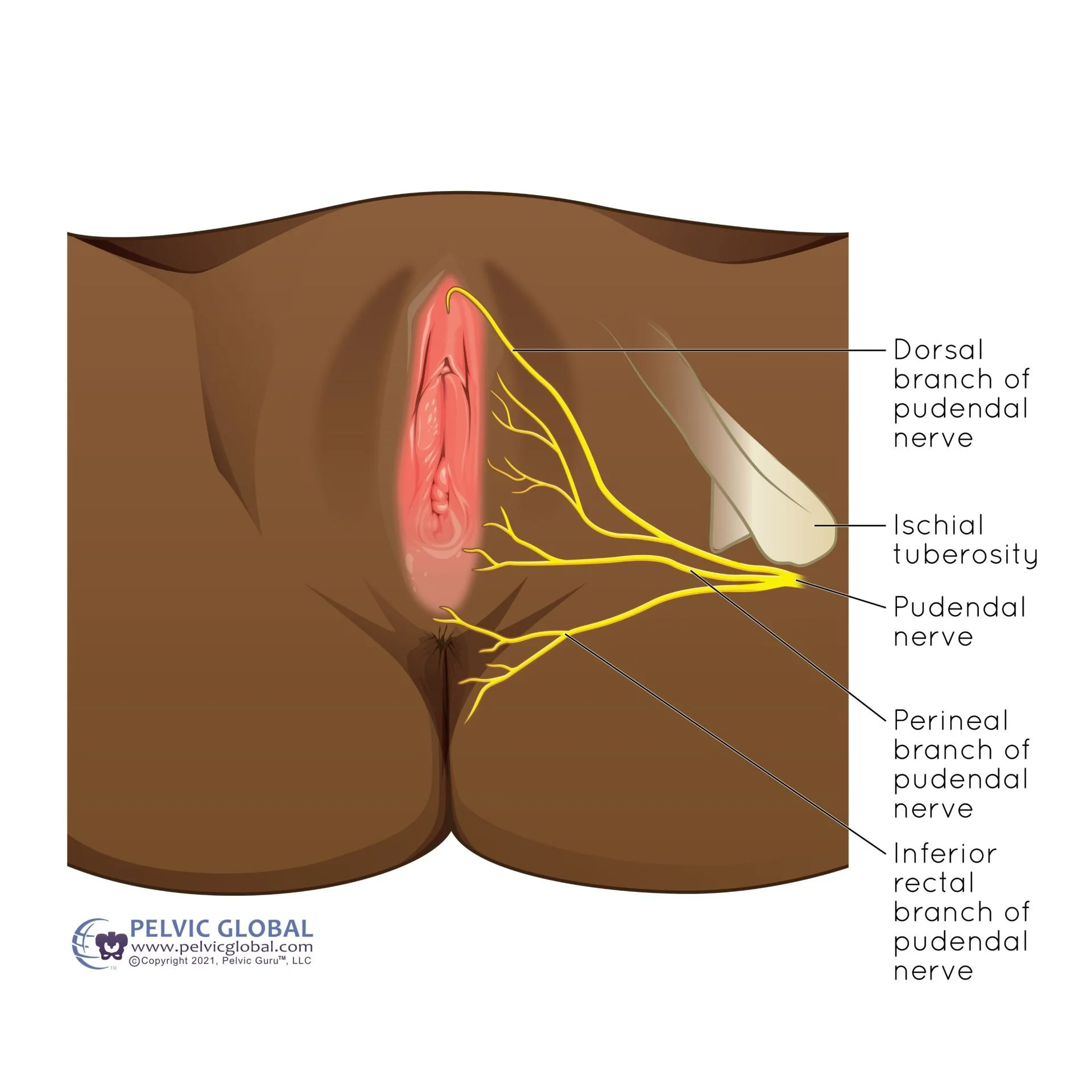
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Sensation Changes:
Numbness or Sensitivity: Nerves are healing and can feel numb or have a heighten sensitivity.
Result: This will improve over time and desensitization techniques can help to tolerate touch.
Improved Comfort: Surgery can help with reduction of symptoms (i.e bulge), discomfort or pain that may have been present prior to surgery.
Result: If any symptoms are persistent, these can be addressed in pelvic floor physical therapy.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Bladder and Bowel Function:
Improve bladder control: reduces symptoms like urinary incontinence, frequency, or urgency.
Improved bowel control: reduces symptoms like straining or emptying.
Result: You gain more confidence with daily activities, exercise and/or social activities. You may have a reduction in embarrassment with needing to assist bowel or bladder movements, improve leakage or pressure.
If either continue post surgery which is common, pelvic floor physical therapy is the first line of defense along with a good bladder and bowel routine.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Scar and Tissue Healing:
Scar Formation: As with any surgery, scar tissue forms at the surgical site. Internal scarring can sometimes cause tightness or discomfort, which might require management through physical therapy or other interventions.
Tissue Healing: Healing of the tissues takes time, you may notice gradual improvements in strength, sensation, and comfort over several weeks to months.
Result: Scar massage or desensitization techniques can improve blood flow and reduce tension around nerves, promoting better healing. Enhanced scar mobility can aid in muscle activation, helping you return to daily life with less pain and discomfort.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Emotional and Physiological Changes:
Confidence and Pain Relief: Surgery helps relieve symptoms that have been limiting your quality of life.
Result: This can lead to increased confidence to return to social events activities, intimate times and physical activities.
Adjustment Period: You may experience an emotional response to re-learning your new body and grieving from possible removal of a pelvic organ.
Result: This can lead to increased self compassion, improved body awareness or body image, and improved daily function leading to a better quality of life.
Lifestyle and Activity Changes:
Activity Restrictions: Initially, you will need to avoid heavy lifting, strenuous activities, and certain movements to protect the surgical repair. Over time, you can gradually return to your usual activities with guidance.
Long Term Care: You may need to adopt lifestyle changes, such as maintaining a healthy weight, avoiding constipation, and practicing pelvic floor exercises, to support the longevity of the surgical repair and prevent recurrence.
Ongoing Monitoring:
Routine Checks Ups: Post-surgery, regular follow-up appointments are essential to monitor healing, address any complications, and ensure that the prolapse repair is holding up well over time.