Section 1:
Introduction to Surgical And Symptom Terms
Understanding Your Pelvic Health Vocabulary
Understanding the language used in pelvic health care can feel overwhelming, especially when you're navigating a new diagnosis, preparing for surgery, or starting physical therapy. This page offers straightforward definitions of the most commonly used terms related to pelvic organ prolapse, pelvic floor muscles, surgical procedures, and common symptoms. These explanations are here to help you feel more informed and empowered in your care journey.
Apical
In the context of prolapse surgery, "apical" refers to the top portion of the vagina — where it connects to the uterus (if present) or the vaginal vault (if the uterus has been removed). So when you hear "apical prolapse," it means that the top of the vagina, uterus, or vaginal cuff is sagging or has lost support.
For Surgery, Apical Procedures aim to restore support to the top of the vagina or uterus and prevent/correct uterine or vaginal vault prolapse.
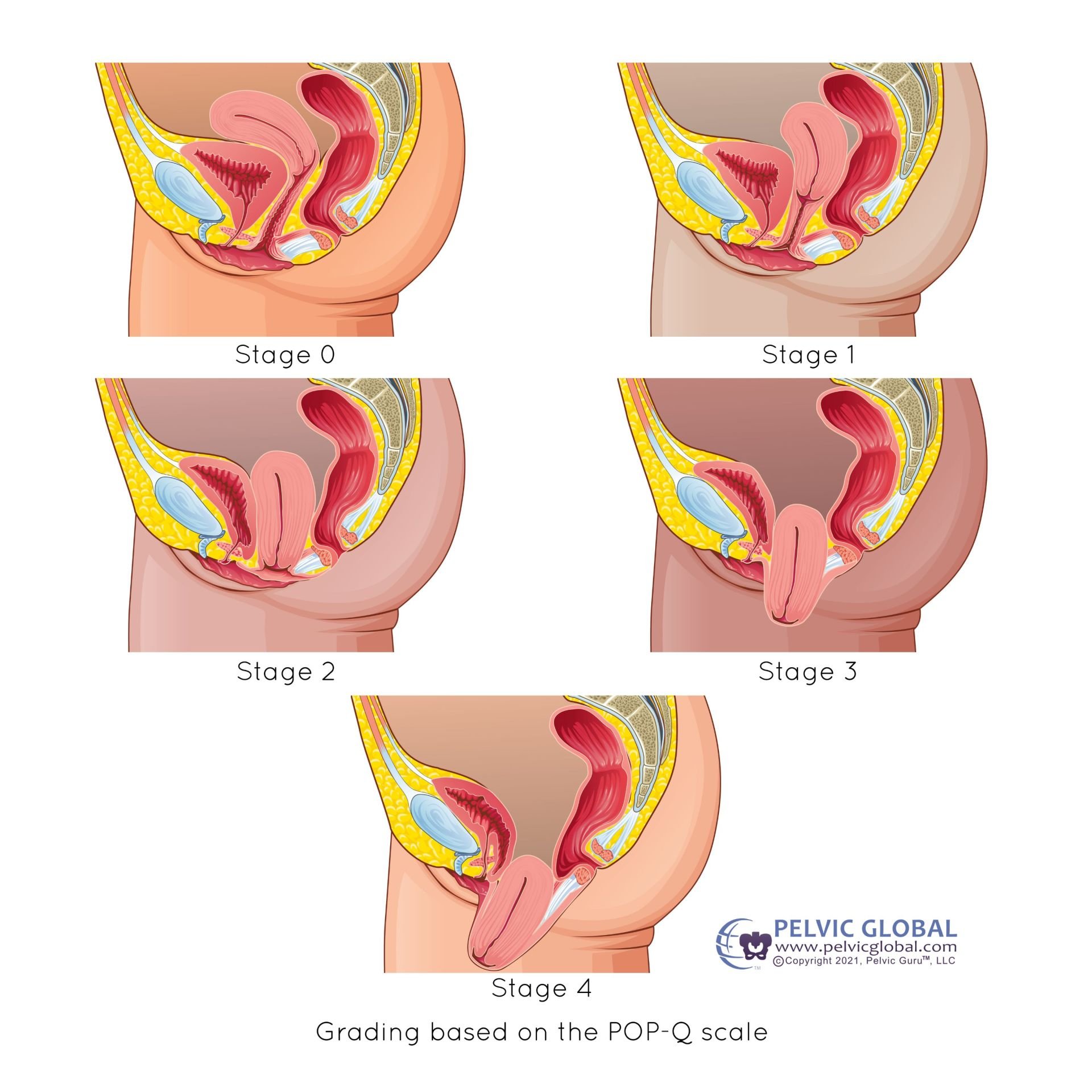
Example of Uterine Prolapse and the various degrees of severity.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Apical prolapse: descent that occurs at the top of the vagina.
Uterine Prolapse: uterus is descent down towards the vaginal opening due to the weakening of the connective tissues take supports the uterus.
Vaginal Vault Prolapse: mid line vaginal wall descends towards the vaginal opening in a women who has had a hysterectomy.
Hysterectomy: A removal of the uterus.
Total Hysterectomy: A removal of the uterus and cervix.
Supracervical Hysterectomy: The uterus is removed, cervix remains.
Sacrocolopopexy: A surgical procedure to correct uterine prolapse or vaginal vault prolapse. This can be performed through an abdominal incision or laparoscopically with or without robotic assistance.
Uterosacral or Sacrospinous Ligament Fixation: A surgical procedure using the person’s own ligaments to suspend to the top of the vagina. This procedure does not use mesh grafts.
Obliterative Procedures: A surgical procedure to narrow and shorten the vaginal opening. This procedure is for a person that does not wish to participate in sexual function with vaginal penetration. There are two types: Partial (Colpocleisis) or Complete (Colpectomy).
Anterior
In the context of prolapse surgery, "anterior" refers to the front wall of the vagina, which lies just behind the bladder. So when someone has an anterior prolapse, it usually means the bladder is bulging into the vaginal wall, a condition called cystocele
For Surgery, Anterior Procedures aim to reinforce the front vaginal wall, support the bladder and correct the cystocele.
Cystocele/Bladder Prolapse: A type of prolapse where the bladder drops into the vaginal wall, causing bladder-related symptoms such as urinary incontinence or frequent urination.
Anterior Repair or Anterior Colporrhapy: surgical procedure that repairs the bladder or bulge from the front (anterior) vaginal wall.
Example of cystocele and the various degrees of severity.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Posterior
In the context of prolapse surgery, "posterior" refers to the back wall of the vagina, which is adjacent to the rectum. A posterior prolapse happens when the rectum bulges into the vaginal wall, a condition called a rectocele
For Surgery, Posterior Procedures aim to repair the back vaginal wall, support the rectum and reduce bulging.
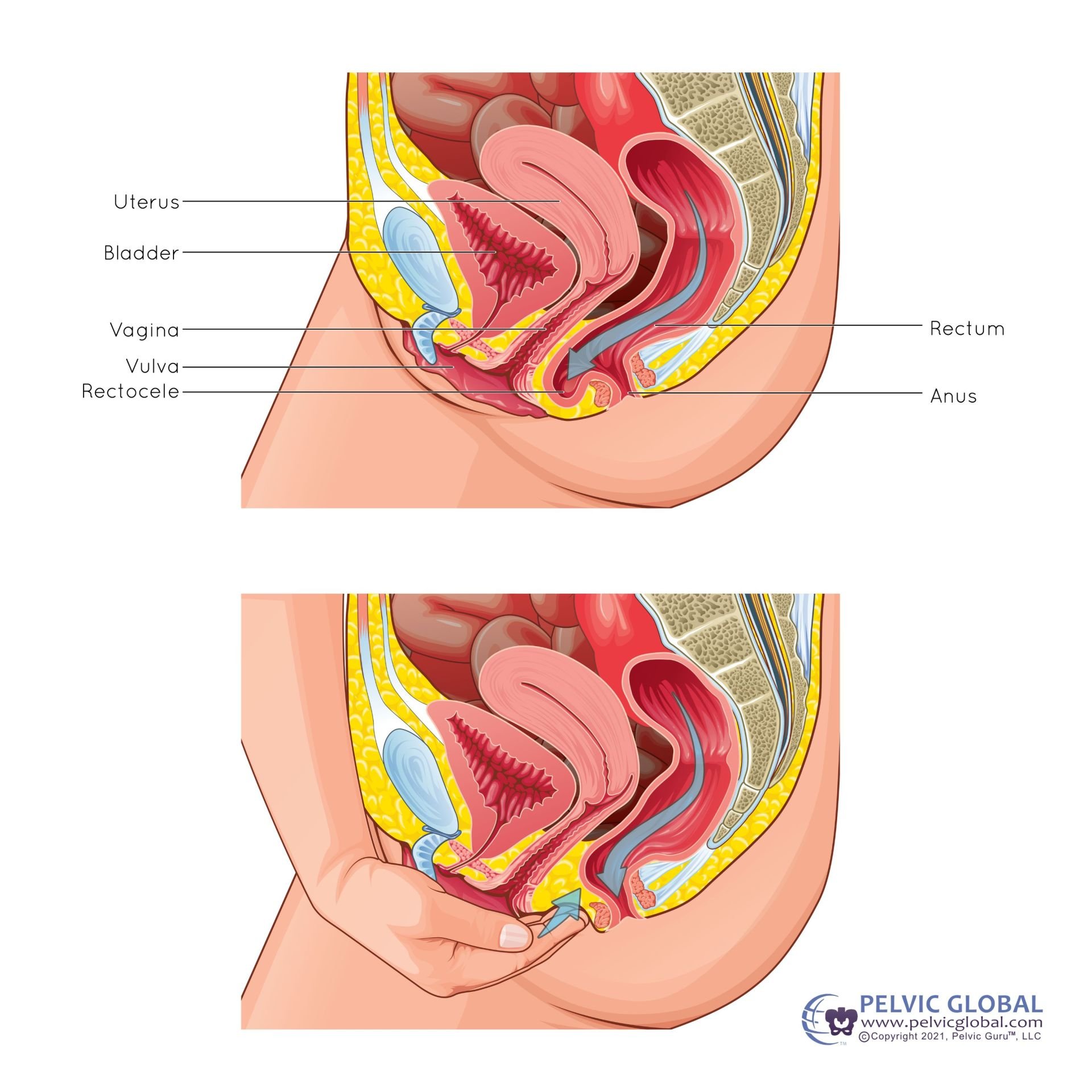
Example of cystocele and the various degrees of severity.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Rectocele/Posterior Wall Prolapse: A type of prolapse where the rectum bulges into the vaginal wall due to weakened pelvic wall tissues or pelvic floor muscles.
Rectal Prolapse: A type of prolapse where the rectum protrudes through the anus.
Posterior Repair or Posterior Colporrhapy: A surgical procedure that repairs the bladder or bulge from the posterior vaginal wall.
Perineorrphaphy: repairing the perineum, the muscles between the anus and vaginal opening.
Common Symptoms of Pelvic Organ Prolapse
Pelvic Pressure or Heaviness
A feeling of something "falling out" or "sitting low" in the pelvis
Worsens as the day goes on or after standing/lifting
Example of a “something coming out” of the vagina
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Bladder Symptoms (anterior prolapse/cystocele)
Urinary incontinence (leakage, especially with coughing or movement)
Incomplete bladder emptying or weak urine stream
Frequent or urgent urination
Incontinence Terms:
Urge Incontinence: A sudden, intense urge to urinate, followed by involuntary bladder contraction and urine leakage.
Stress Incontinence: A type of incontinence caused by pressure on the bladder, such as during coughing, sneezing, or exercise, often due to weakened pelvic floor muscles.
Mixed Urinary Incontinence: A combination of the above terms.
Overactive Bladder: Urinary urgency with frequency, night time urination and sometimes leakage without an infection.
Example of splinting technique to help defecation
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Sexual Symptoms
Discomfort or pain during intercourse
Decreased sensation
Self-consciousness about bulging
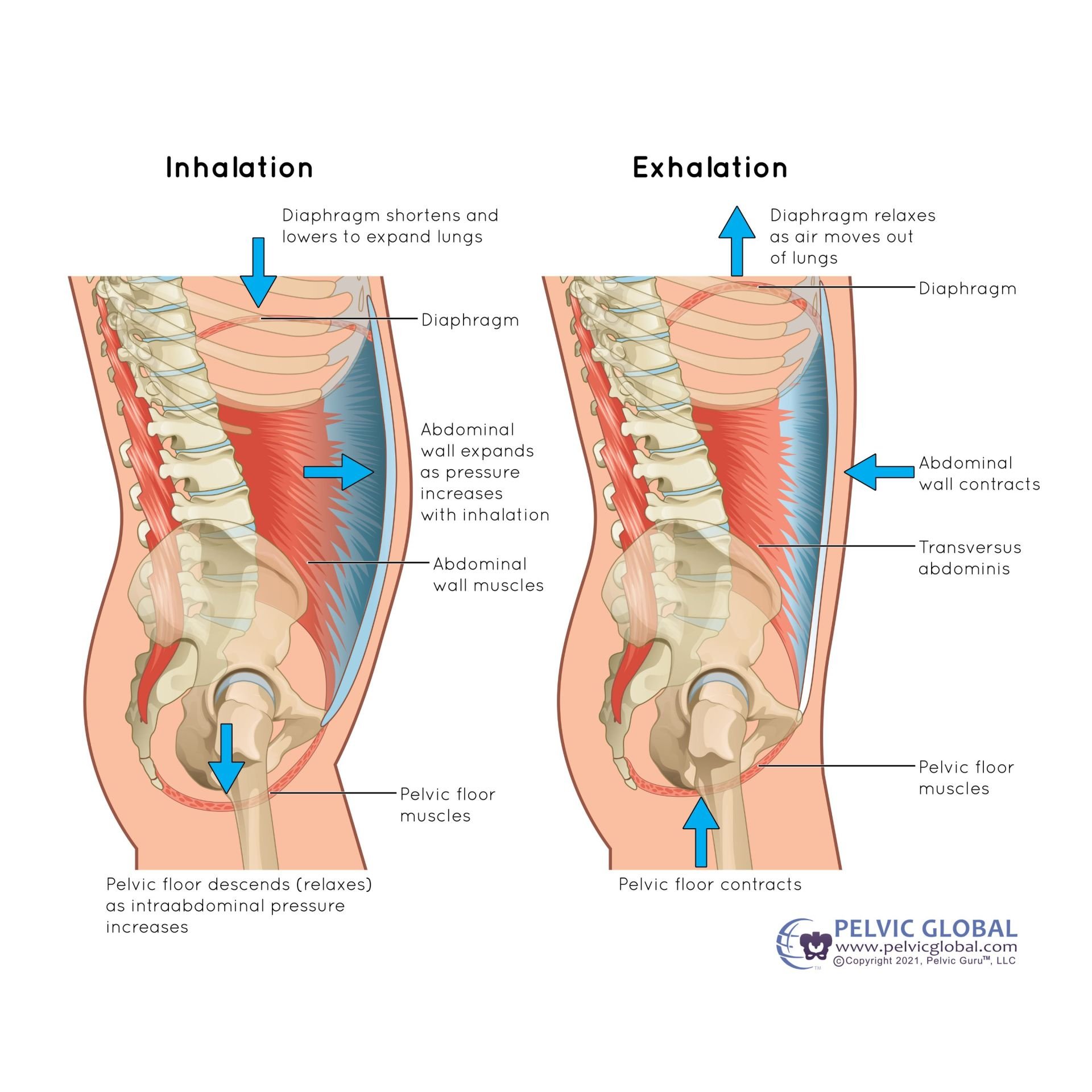
Example of core cainster including the low back to demonstrate how this is connected to the pelvic floor muscles and cavity
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Summary of Pelvic Organ Prolapse Symptoms:
Some women with mild prolapse may have no symptoms at all
Symptoms often worsen with prolonged standing, lifting, or straining
Prolapse is dynamic and will change throughout the day and/or with activity
Symptom severity is based on the individual and how is affects their life
Examples of different types of pelvic organ prolapse that can cause a sensation of “falling out” or “sitting low”
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Vaginal Bulge or Protrusion
A visible or palpable bulge at or beyond the vaginal opening
Many women describe it as “something coming out” of the vagina
Example of bladder filling and emptying; Prolapse can affect this process
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Bowel Symptoms (posterior prolapse/rectocele)
Difficulty having bowel movements
Need to press on the vaginal wall to assist with defecation (called “splinting”)
Feeling of incomplete evacuation
Example of dilator technique to help reduce muscle tension
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Low Back or Pelvic Pain
Achy or dragging pain in the lower back, especially later in the day
Pelvic Floor Muscles
The pelvic floor muscles are a group of muscles that form a hammock-like structure at the bottom of the pelvis. They support the pelvic organs (bladder, uterus or prostate, and rectum), and play a crucial role in urination, bowel movements, sexual function, and core stability.
Main Pelvic Floor Muscles:
These are often grouped together and referred to as the levator ani and coccygeus muscles.
Levator Ani Group (the main support muscles)
Pubococcygeus
Puborectalis
Iliococcygeus
Coccygeus (also called ischiococcygeus)
Smaller, more posterior muscle helping stabilize the tailbone.
Functions of Pelvic Floor Muscles:
Support the bladder, uterus/prostate, and rectum
Control continence (by contracting to prevent leaks)
Relax to allow urination, bowel movements, and childbirth
Contract during sexual activity (pleasure and stability)
Work with your core muscles for posture and stability
A Kegel contraction is the intentional tightening and lifting of the pelvic floor muscles — the same muscles you use to stop the flow of urine or hold in gas.
What Happens During a Kegel Contraction:
The pelvic floor muscles contract (squeeze inward and upward)
The urethra, vagina, and rectum are gently lifted and supported
It helps close openings to prevent leaks from the bladder or bowel
How to Do a Basic Kegel:
Imagine you're stopping the flow of urine or holding in gas — that's the right set of muscles.
Squeeze and lift those muscles
Hold for 3–5 seconds, then relax completely for the same amount of time.
Repeat for several reps, a few times a day.
Tips:
Think of the muscles as an elevator: Close the doors (aka squeeze the holes) and lift the elevator up 1-2 floors
Blow through a skinny straw when performing a kegel - see image
Important Notes:
Don't actually practice during urination regularly — that can confuse your bladder signals.
Avoid squeezing your glutes, inner thighs, or abs — it should feel internal and subtle.
Kegels should feel like a gentle lift, not a downward push.
Illustration of Pelvic Floor Muscles looking from top down
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)Breathing mechanics for when performing a kegel
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)